A pioneering approach of focusing solely on healthcare system as our dedicated sector and delivering value through creative solutions.
- billing@thedocsxpress.com
- Mon - Fri : 09:00 to 18:00
Any Questions? Call us
The demographics of patients are the basis for all medical data. Information such as: Patient name, Date of birth, Address, Phone number, Doctor Information, Social Security number (SSN) and gender is collected during the registration process. In the patient’s medical record, the demographics section contains information about his or her guarantors and emergency contacts, as well as health insurance. This is necessary since the accuracy and quality of the data will directly affect the physician’s monthly revenue. Also known as the charge sheet or claim, it is an important part of the billing process.
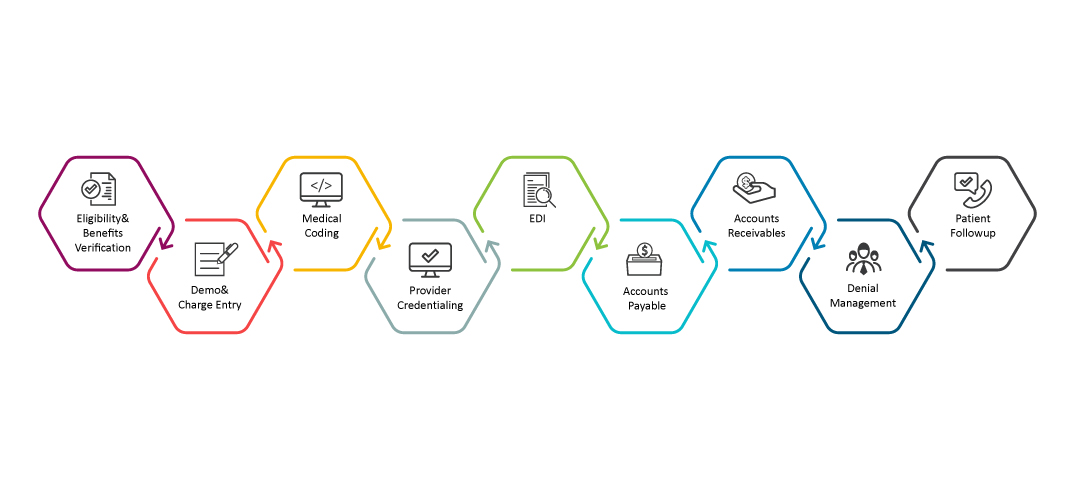
A medical coding and billing process begins with insurance verification. As the healthcare industry continues to change and become more complex, more than ever it is essential to validate coverage, benefits, co-payments, and deductibles. A successful eligibility verification is essential to successful billing. By verifying the patient has active coverage on the date of service, and that his or her insurance plan covers the services provided, the provider can be assured that these services will be paid for. As a result, providers of medical care must be aware of the importance of insurance verification in the healthcare industry.
The process of medical coding is similar to translation. In order to correctly code the patient’s medical chart, the medical coder needs to understand/read the encounter notes. In this section, the history, diagnosis, treatment, and course of action are outlined. This information must be converted into universal medical codes. Current Procedural Terminology (CPT®) and Healthcare Common Procedure Coding System (HCPCS) codes are available from the AMA to help accurately bill procedures and services. Currently, the ICD (10th revision) is being used for coding.
It involves the process or set of processes that are used to submit charges for medical procedures and other patient-facing services to payers for billing. As part of this process, a detailed accounting of services rendered is completed, as well as initial information gathering. Every medical procedure is updated with new charges and codes on a regular basis. As per the schedule, the Specialist will compile billing information, assist with coding and assign the appropriate fees.
Billing and Submission of Claims- Once a claim has been properly filled out, the claim must be submitted to the insurance company for payment. In order to submit claims in a timely manner, medical billers must have access to the information they need concerning the insurance payers since each insurance payer has a number of variables that impact how and when to submit claims.
Provides accurate posting of payments from third-party carriers and patient payments. Accounts’ rejection notices from third-party carriers are posted/documented in this section. Ensures that payments posted to billing system are reconciled with the payment batch each day and corrects any discrepancies. Makes adjustments and posts payments to the appropriate patient invoice. Identifies issues with payment amounts. Compiles ERA files and EOBs with the corresponding EFTs and paper checks.
A healthy cash flow and successful revenue cycle management are dependent on effective denial management. If you fail to handle denials from insurers adequately, you will lose revenue for your practice. By analyzing the possible denial trends, our experts initiate a ‘global action’ that will have an impact on many claims with a simple fix to prevent repetition of the same denials.
All healthcare providers have accounts receivable services as a significant asset. Our billing and collections activities comply with all state and federal laws. Utilize monthly aging reports to keep track of unpaid claims and file appeals when necessary for maximum reimbursement. Responsible for reducing outstanding receivables by following up on assigned accounts in a timely manner.
The process of credentialing and enrollment is crucial to business operations. Credentialing takes place at both the provider and payer level. It entails examining a provider’s qualifications and practice history as part of the credentialing process. As a provider, Enrollment refers to the process of requesting to be included in a network of health insurance providers. Obtaining enrollment with or a contract with a plan/network is part of the provider enrollment process.
Enter your email address to get latest updates and offers from us. Also some Discount coupons.

